Tool: Telehealth Policy Finder
-
Focus Areas
Data, Technology & Innovation -
Issues
Technology & Telehealth -
Programs
Center for Connected Health Policy
Across the country, no two states are alike in how they define and regulate telehealth. To help policymakers, health advocates and other health care professionals understand the policies and trends throughout the nation, the Telehealth Policy Finder tool compiles telehealth-related laws and regulations across all 50 states and the District of Columbia, as well as at the federal level.
Explore the Policy Finder toolFall 2024 Updates
As some states have implemented targeted exceptions from licensing requirements for out-of-state telehealth providers since Fall 2023 (as discussed above), other states have implemented special registrations or licensure processes for out-of-state telehealth providers, allowing an alternative process to full in-state licensure to offer telehealth services within the state in certain instances and subject to specific requirements. Twenty-two states, as well as the Virgin Islands now offer special telehealth licenses, or registration processes for out-of-state providers. To be counted in this number, the licenses/registrations did need to specifically reference telehealth (or remote care) in some way. A recent state to implement this is Arizona, which introduced new regulations (implementing a previously passed law) that establishes a telehealth provider registration process for out-of-state providers, outlining practice standards such as consent and liability insurance requirements within it. In Washington, SB 5481 enacted the Uniform Telehealth Act, which in addition to adopting limited licensure exceptions for out-of-state providers, encourages a review of the Uniform Law Commission’s proposal for an out-of-state provider registration process, signaling the state’s interest in developing a more formalized approach. Delaware also adopted regulations that allow social workers practicing via interstate telehealth to bypass the need for a full Delaware license if they are registered under the state’s telehealth registration system.
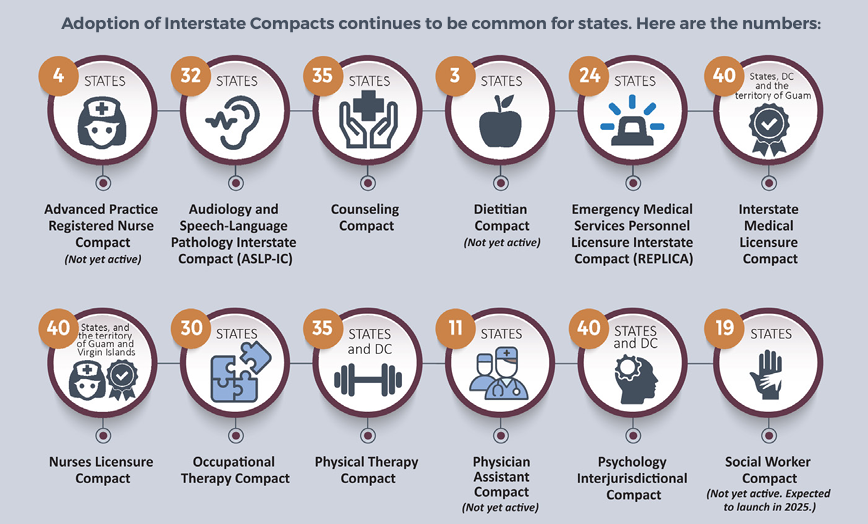
Although states have introduced specific provisions for out-of-state providers, interstate compacts remain the most common method for enabling out-of-state practitioners to work across multiple professions and states. These compacts typically allow specific healthcare providers to practice in states where they are not licensed, provided they hold a valid license in their home state, and possess a special ‘compact’ license. Currently, CCHP monitors twelve different Compacts, each with its own distinct eligibility criteria and process. For instance, the Interstate Medical Licensure Compact streamlines the licensure process, although physicians are still required to apply for licenses in individual states. We saw the largest jump in participation in the Social Work Compact, Counseling Compact and Physician Assistant Compact during this Fall 2024 edition of the report. Since last year, a new Compact was also added to CCHP’s tracking, the Dietitian Compact. So far, only three states (Alabama, Nebraska and Tennessee) are member states. In addition, as some compacts are relatively new, not all are currently considered active and/or issuing licenses at this time.
Read the full Fall 2024 report, and explore the state summary chart showing where states stand on many key telehealth policies, as well as an infographic highlighting key findings.
Additional findings:
- Fifty states, Washington DC and Puerto Rico provide reimbursement for some form of live video in Medicaid fee-for-service. The Virgin Islands does not explicitly indicate they reimburse for live video in their permanent Medicaid policies.
- Thirty-seven state Medicaid programs reimburse for store-and-forward. Colorado, Delaware, New Hampshire, and Pennsylvania are the states which added reimbursement for store-and-forward, although each in a limited capacity. Note that some states only reimburse store-and-forward through specific communication technology-based service (CTBS) codes.
- Forty-two state Medicaid programs provide reimbursement for remote patient monitoring (RPM). Five states, (Delaware, New Hampshire, New Jersey, Pennsylvania and South Dakota) added reimbursement for RPM since Fall 2023.
- Forty-five states and DC Medicaid programs reimburse for audio-only telephone in some capacity; however, often with limitations. Two states, Delaware and West Virginia, added reimbursement for audioonly telehealth in some capacity since Fall 2023.
- Thirty-one state Medicaid programs including Alaska, Arizona, California, Colorado, Delaware, Hawaii, Illinois, Iowa, Kentucky, Maine, Maryland, Massachusetts, Michigan, Minnesota, Missouri, New Hampshire, New York, North Carolina, North Dakota, Ohio, Oregon, Pennsylvania, South Carolina, South Dakota, Texas, Utah, Vermont, Virginia, Washington, West Virginia, and Wisconsin reimburse for all four modalities (live video, store-and-forward, remote patient monitoring and audio-only), although certain limitations may apply.
- Forty-four states, the District of Columbia, Puerto Rico and the Virgin Islands have a private payer law that addresses telehealth reimbursement. Not all of these laws require reimbursement or payment parity. Twenty-three states have explicit payment parity. Both Puerto Rico and Pennsylvania are the two new states that have added private payer policies since Fall 2023.
- Forty-seven states, DC, and Puerto Rico include some sort of consent requirement in their statutes, administrative code, and/or Medicaid policies. South Dakota and Montana added consent requirements since Fall 2023.
- Thirty-eight states, as well as DC offer some type of exception to licensing requirements. Note that while CCHP’s search of statute and regulations was confined to telehealth, if we happened to come across a more general licensing exception, we did include it in our reporting, and in this number. CCHP also found that twenty-two states as well as the Virgin Islands have telehealth-specific special registration or licensure processes as an alternative to full licensure for certain providers or as an additional requirement to utilize telehealth. To be counted in this number, the licenses/registrations did need to specifically reference telehealth (or remote care) in some way.
- Many states continue to implement telehealth practice requirements for various professions. While the majority of states have telehealth practice standards in place for certain providers, such as physicians and mental health professionals, more state boards are starting to adopt professional standards for other types of practices, for example acupuncture providers and dietitians.
- While CCHP doesn’t keep specific counts of states with prescribing requirements (because there are so many caveats and exceptions), we do include it as a category under Professional Requirements in our Policy Finder. Since Fall 2023, several states have implemented new rules around prescribing via telehealth, especially for controlled substances.

Out-of-State Policy Trend Map
CCHP has added an Out-of-State Telehealth Providers policy trend map to the CCHP website which color codes states based on the presence of limited licensure exceptions, telehealth registration processes, or both. This webpage also provides a link to CCHP’s Interstate Licensure Compacts information, showing Compact participation status by state.
Getting started with the Policy Finder
Launched in Spring 2021 by PHI’s Center for Connected Health Policy (CCHP), the Policy Finder tool is a searchable, easy-to-use database that is updated consistently throughout the year. Formerly known as the State Telehealth Laws and Reimbursement Report, the information from the online database can be exported for each state into a PDF document using the most current information available on CCHP’s website.
Use the Policy Finder tool to:
- Look up telehealth-related laws and regulations by topic, including COVID-19, Medicaid & Medicare, Private Payer and Professional Requirements
- Explore all current laws, temporary COVID-19 actions, and pending legislation in all 50 states and the District of Columbia, as well as at the federal level
- Compare the policy of any of the topic areas for any two states
- View color-coded maps recapping policy trends by state across topic areas, including Medicaid reimbursement for live video, store and forward and remote patient monitoring
The Policy Finder is designed to provide timely policy information that is easy for users to navigate and understand. Watch a quick tutorial to explore the tool, see how to use it and learn about its features:
Please note: this information should not be construed as legal counsel. Consult with an attorney if you are seeking a legal opinion.
Originally published by Center for Connected Health Policy
Work With Us
You change the world. We do the rest. Explore fiscal sponsorship at PHI.
Support Us
Together, we can accelerate our response to public health’s most critical issues.
Find Employment
Begin your career at the Public Health Institute.