Supporting Communities and Local Public Health Departments During COVID-19 and Beyond: A Roadmap for Equitable and Transformative Change
-
Focus Areas
Capacity Building & Leadership, Communicable Disease Prevention, Healthy Communities -
Issues
Workforce Development -
Programs
Public Health Alliance of Southern California -
Strategic Initiatives
COVID-19, Vaccine Access & Equity

In response to the COVID-19 pandemic, California and the nation are poised to transform their systems in a way that was not possible before, to advance an equitable and just future for all communities. Transitioning from short-term crisis response to longer-term recovery, provides a unique moment to catalyze transformative action to reimagine and rebuild systems, strengthen communities, and redefine social contracts with community resilience and equity at the core.
The transformation will require co-visioning, and co-creating with community leaders and members to ensure that as California rebuilds its systems, the needs and priorities of communities most disproportionately impacted by inequities are the driving force and pillars of our reimagined systems.
The California Department of Public Health’s Office of Health Equity contracted with the Public Health Alliance of Southern California (Public Health Alliance) to produce this report with policy, program, and resource recommendations, and best practice examples, ensuring that local public health departments (LHDs) are adequately prepared to protect communities most vulnerable to the health and socioeconomic impacts of COVID-19 as well as future public health emergencies.
This report elevates best practices, including local public health department, community-based, healthcare, and philanthropic efforts, to support communities most vulnerable to the impacts of COVID-19 throughout the response and recovery process.
Download the executive summary
Key Findings
- 87% of LHD respondents said knowledge of community engagement and partnerships was the most critical staff skill in the COVID response. (November 2020 LHD Survey Results)
- When the pandemic unfolded in early 2020, LHDs were already underfunded for their core functions. When they quickly had to pivot to address the growing threat of COVID-19, 89% stated that funding was a barrier to addressing the response, with a quarter stating it was a major barrier. (November 2020 LHD Survey Results)
- 59% of respondents indicated that they do not have funded equity staff – of those, 83% believe additional funding for dedicated equity staff would have better supported their department’s COVID response. (November 2020 LHD Survey Results)
- 85% of CBOs indicated that they would most benefit from general operating support in order to make the greatest impact during COVID-19 and other public health and climate emergencies. (November 2020 CBO Survey Results)
- State and federal decisions have led to California’s LHDs receiving $177 million less in total funding in 2018-2019 versus 2007-2008. This mirrors national trends: Over the past decade alone, local and state health departments across the country lost 20% of their workforce, and LHD budgets shrank by as much as 24%.
Recommendations
This report is broken down into seven key content areas that emerged through in-depth interviews, surveys, and practice and policy scans over the past year with diverse stakeholders, including: public health professionals and data experts, community-based organizations and advocates, healthcare systems and health plans, philanthropic groups, and labor organizations.
- Bolster Investments in Public Health Departments and Communities to Advance Health Equity
- Build a Resilient Equity-Focused Local Public Health Workforce for the 21st Century
- Embed Equity throughout Local Public Health Department Emergency Planning, Response and Recovery
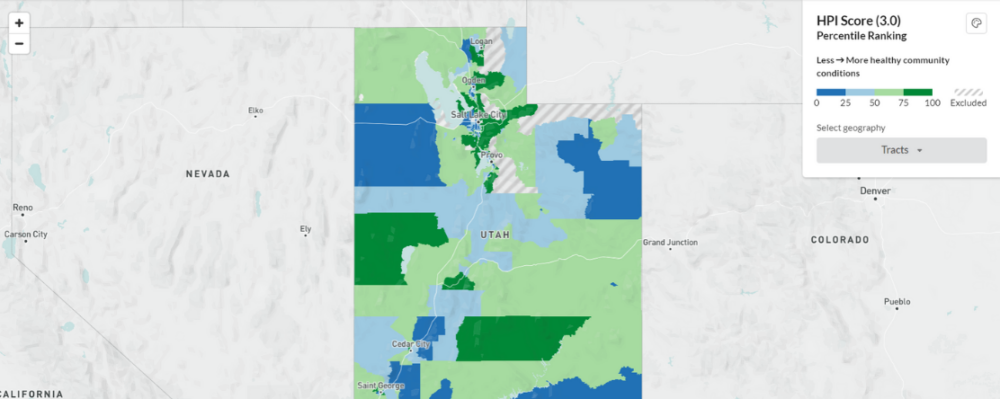
- Catalyze Transformative Shifts in Utilizing Data
- Advance Health Equity and Strengthen Resilience through Ongoing Community-Informed Policy and Practice Changes
- Ensure Greater Coordination, Collaboration, and Consideration of Equity Impacts when Issuing Health Orders and Guidance
- Build Effective, Actionable Partnerships between Local Public Health and Healthcare Systems
Each section includes high level framing, challenges that influenced the COVID-19 emergency response and recovery, best practices, and a mixture of practical, short-term recommendations, and long-term guidance to address structural issues.
“It is essential to recognize that the choices made today will have lasting implications on the public’s health and the ability to advance healthier, equitable communities tomorrow. The pandemic may be a once-in-a lifetime event, yet there are many other health inequities and racial injustices occurring on a daily basis that systems need to be prepared to prevent and protect those most likely to be impacted. It is important to invest in communities and systems in ways that enable everyone to live to their full potential, where people have stability and security in their work, homes, schools, and environment to enjoy life, and where all sectors come together to help each other and ensure no one is left behind.” – Supporting Communities and Local Public Health Departments During COVID-19 and Beyond: A Roadmap for Equitable and Transformative Change
Work With Us
You change the world. We do the rest. Explore fiscal sponsorship at PHI.
Support Us
Together, we can accelerate our response to public health’s most critical issues.
Find Employment
Begin your career at the Public Health Institute.