A Decade of Advancing Telehealth Policy: PHI’s Center for Connected Health Policy
Highlights

In their first decade, PHI’s Center for Connected Health Policy has taken on a critical role as the federally designated National Telehealth Resource Center for Policy, helped advance multiple telehealth policies over the years, navigated drastic changes during COVID and more.
10 years advancing state and national telehealth policies that promote better systems of care and improved health outcomes, as well as provide more equitable access to quality, affordable health care and services.
-
Focus Areas
Health Care & Population Health -
Issues
Technology & Telehealth -
Expertise
Public Policy Advocacy
PHI’s Center for Connected Health Policy (CCHP) acts as a catalyst for change by providing nonpartisan, unbiased, and research-based analyses, reports and telehealth resources to policy makers, the private healthcare sector, health plans, academic researchers, and consumer health advocates.
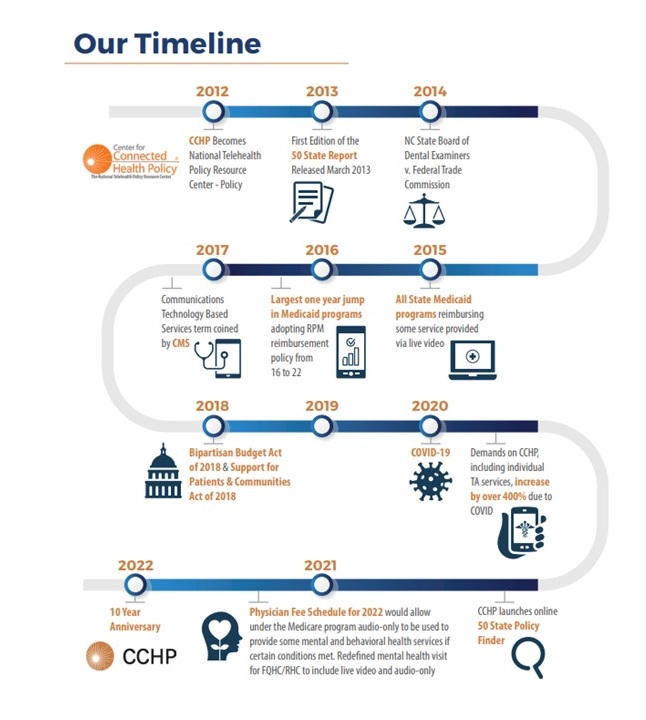
For over a decade, PHI’s Center for Connected Health Policy (CCHP) has advanced state and federal telehealth policies to help improve greater access to healthcare for patients across the nation. Here are some of the greatest successes they’ve had over the past 10 years:
- In 2009, before most really understood what telehealth was, CCHP launched the Specialty Care Safety-Net Initiative where CCHP used telehealth to connect patients in rural and urban medically underserved communities with specialists in six high-need disciplines at University of California Schools of Medicine. This 3-year telehealth demonstration project connected 43 safety-net health centers across California with specialists at five University of California Medical Centers.
- In 2012, CCHP was selected as the federally designated National Telehealth Resource Center for Policy and transitioned quickly from their work in California to covering the entire nation. By Fall 2022, CCHP was tracking policies for all 50 states, the District of Columbia, Puerto Rico, the Virgin Islands, and federally.
- In 2020, during the onset of the COVID-19 pandemic, CCHP successfully navigated what can only be described as a tsunami of telehealth policy changes, on both the federal and state level. CCHP was constantly dealing with a deluge of changes from 52 different jurisdictions (50 states, DC and the federal government). During this time period, CCHP issued nearly four times the number of notices and analyses of telehealth policy changes than in a typical year for that same period of time, helping to keep the nation informed on state and federal telehealth policy changes during a time of instability and confusion.
How It Began
Established in 2008 with funding from the California Health Care Foundation, CCHP’s work was originally focused exclusively on California telehealth policy. In 2011, the team published the Telehealth Model Statute Report, which became the basis for the California Telehealth Advancement Act of 2011 (AB 415) and cemented CCHP’s position as experts in telehealth policy.
In 2012, CCHP applied for and was awarded federal funding by the U.S. Health Resources and Services Administration (HRSA) to be the federally designated National Telehealth Resource Center for Policy, tracking policy development in all 51 jurisdictions in the United States and at the federal level. This allowed for an incredible and unique opportunity to study the development of telehealth policy and the opportunity to be a part of some of the most significant telehealth policy advancements in the U.S.
The CCHP team transitioned quickly from a statewide program to offering key support to 12 regional telehealth resource centers and serving as a National Telehealth Resource Center for Policy. This transition allowed for CCHP to demonstrate its ability to serve as a powerful convener, investigator, resource, and change-maker across different spaces within the telehealth world. Today, CCHP also continues to advance California’s leadership in telehealth policy, and heads up the California Telehealth Policy Coalition, a group of over 160 member organizations including consumer groups, medical systems, payers, providers, and technology representatives.
Setting a Framework for State & Federal Efforts
As the federally funded National Telehealth Resource Center for Policy, CCHP had a key opportunity to create the first-ever 50 State telehealth laws and reimbursement policies report, a compilation of all state telehealth Medicaid policies, laws and regulations.
CCHP staff developed a strategic approach and research framework for the project and based on surveys and interviews, 11 categories were identified as focus areas for the telehealth 50 State project. These categories were:
- Definition of Telehealth/Telemedicine
- Reimbursement for Live Video
- Reimbursement for Store and Forward
- Reimbursement for Remote Patient Monitoring (RPM)
- Reimbursement for Email/Phone/Fax
- Consent
- Location
- Transmission/Facility Fees
- Online Prescribing
- Private Payer Laws
- Licensure
The 50 State project was able to help establish a baseline for state telehealth policy to compare subsequent years and watch how policy evolves over time. Using this framework, CCHP has found that there has been significant progression in adopting telehealth policies over the past decade.
Federally, much of CCHP’s telehealth efforts focused on Medicare, where the largest development of telehealth-specific policy enacted by the federal government exists. Over the years, CCHP has also examined the use of federal telehealth policy to prescribe controlled substances – also known as the Ryan Haight Act, and examined the Health Insurance Portability and Accountability Act of 1996 (HIPAA). The Ryan Haight Act details extremely limited circumstances when the use of telemedicine is allowed to prescribe controlled substances, generating many questions from providers. In contrast, HIPAA has no language specific to telehealth, and the Health and Human Services (HHS) Office of Civil Rights (OCR) only recently (June 2022) released guidance on remote communication technology to help providers understand their obligations.
How the COVID-19 Pandemic Changed the Telehealth Landscape
In 2020, when the COVID pandemic was declared a national public health emergency, telehealth policy on a state and federal level changed drastically. While most of the nation had to severely limit their interactions, the healthcare system still had to find a way to meet the critical needs of patients, while limiting contact and the spread of COVID from face-to-face visits. It was at this point that telehealth was looked to as a critical solution to meeting some of these needs.

At the time, the policy environment did not allow for widespread use of telehealth, particularly if patients were in non-traditional medical locations such as the home, where most people were in the early days of the pandemic. Medicare was also extremely limited in what was allowed, causing greater concern as the population covered by the Medicare program were some of the most vulnerable to COVID-19. This led to what can only be described as a tsunami of telehealth policy changes, on both the federal and state level.Mei Kwong, JD
Executive Director
As an organization tracking telehealth policy on the federal and state levels, CCHP was at the forefront and constantly dealing with a host of changes from 52 different jurisdictions (50 states, DC and the federal government). In just a few months (March – May 2020), CCHP issued almost four times the number of notices and analyses of telehealth policy changes than what is typically completed in a year for that same period of time.
One of the major policy developments during the COVID pandemic was the increased allowance of providers using audio-only telehealth services. During pre-pandemic times, audio-only services were not considered allowable under telehealth in many jurisdictions. The pandemic shed light on the digital divide and that many community members lacked access to internet or other capabilities such as live video. CCHP has compiled a full list of the federal changes and COVID-19 policies for each state.
Telehealth in the Time of COVID: What Comes Next
During the early onset of the COVID pandemic, many states had to move quickly to put temporary telehealth policies in place. Now, as many of the temporary policies put into place begin to expire, state and federal legislators are grappling with three possible approaches to address the future of these temporary policies:
- Allow the policies to lapse and return to pre-pandemic policies
- Adopt some or all of the temporary policies permanently
- Extend the temporary policies (all or some) to a future point in time (i.e. June 2023)
As of September 2022, more than half of the jurisdictions (35) have enacted audio-only telehealth policies in Medicaid programs. The telehealth policy landscape is ever-changing and impacted by the world around us and current events, some not directly related to telehealth, but with vast implications on how to provide quality healthcare to community members across the U.S.
CCHP welcomes the dynamic nature of this work. Telehealth policy operates within a multi-faceted and highly complex environment where a simple answer may not be available for many questions. As these policies continue to evolve on both the federal and state level, CCHP will continue the work it has done over the past decade for as long as possible.Mei Kwong, JD
Executive Director
Learn More: Explore the National Telehealth Resource Center for Policy 10-Year Anniversary Report
Released in Fall of 2022, The National Telehealth Resource Center for Policy 10-Year Anniversary Report is a celebration of how far CCHP has come as the federally designated National Telehealth Policy Resource Center and the overall contributions that they’ve made to the field of telehealth. The report captures some of the highlights, significant changes and environmental factors that have had an impact on shaping telehealth policy development throughout the nation. It also provides a glance at how telehealth policy came to be what it is today.
The 10-Year Anniversary Report honors the memory of Mario Gutierrez, who was the CCHP’s executive director from 2011-2017 and whose vision in 2012 led CCHP to apply for and serve as the National Telehealth Policy Resource Center.
Center for Connected Health Policy Staff Over the Years
Work With Us
You change the world. We do the rest. Explore fiscal sponsorship at PHI.
Support Us
Together, we can accelerate our response to public health’s most critical issues.
Find Employment
Begin your career at the Public Health Institute.