Promoting Safer Pregnancies
Highlights

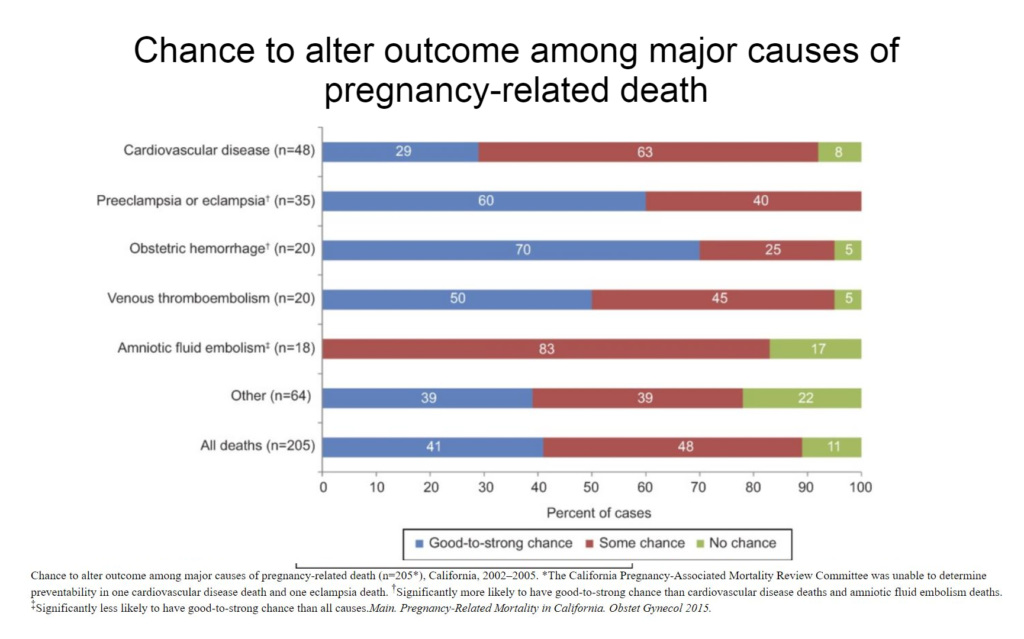
PHI researchers and their partners produced the Pregnancy-Associated Mortality Review to address maternal mortality, finding an overall 41% good-to-strong chance to alter the outcome in pregnancy-related deaths.
70% of deaths in pregnancies due to hemorrhage had a good-to-strong chance of being prevented
60% of deaths in pregnancies due to preeclampsia had a good-to-strong chance of being prevented
-
Issues
Reproductive & Sexual Health
In the United States, death rates during pregnancy have fallen from 850 in 1900 to fewer than 8 per 100,000 in 1997. But in the past twenty years, this trend has been reversing, with pregnancy-related mortality more than doubling, to 17.8 per 100,000 live births.
In 2015, researchers from the Public Health Institute, the California Department of Public Health, and the California Maternal Quality of Care Collaborative at Stanford University produced the Pregnancy-Associated Mortality Review to address maternal mortality. While previous studies typically looked at a single cause of pregnancy-related mortality, with limited access to clinical information and few recommendations for improving outcomes, PHI’s collaboration used full medical records from women in California between 2002–2005 whose deaths were related to their pregnancies to assess the five leading causes of mortality and identify areas where hospitals and providers could make improvements.
The study found an overall 41% good-to-strong chance to alter the outcome in pregnancy-related deaths, including:
- A good-to-strong chance of preventing death was found in 70% of hemorrhage deaths and 60% of deaths from preeclampsia.
- A good-to-strong chance of preventing death was found for 29% of deaths from cardiovascular disease, which was the most common cause of pregnancy-related death.
- Another 63% of cardiovascular deaths were found to have some chance of being preventable.
The study also found that health care provider factors were the most common type of contributor identified for all five leading causes of death, with the most common factors being delayed response to clinical warning signs and ineffective care.The findings underscore the need for public health interventions and support for hospital, state, and national maternal health and safety programs.
See the study in the journal Obstetrics and Gynecology and see more here.
Work With Us
You change the world. We do the rest. Explore fiscal sponsorship at PHI.
Support Us
Together, we can accelerate our response to public health’s most critical issues.
Find Employment
Begin your career at the Public Health Institute.
