In the News
Many ERs Fail People Who Struggle With Addiction. These New Approaches Might Help
- National Public Radio
-
Focus Areas
Alcohol, Tobacco, Drugs & Mental Health -
Programs
CA Bridge -
Strategic Initiatives
Opioids

For years, Kayla West watched the opioid epidemic tear through her eastern Tennessee community. As a psychiatric nurse practitioner, she treated people with mental illness but felt she needed to do more to address addiction.
So in 2020, when the state created a position to help hospitals improve addiction care in the emergency room, West jumped at the opportunity.
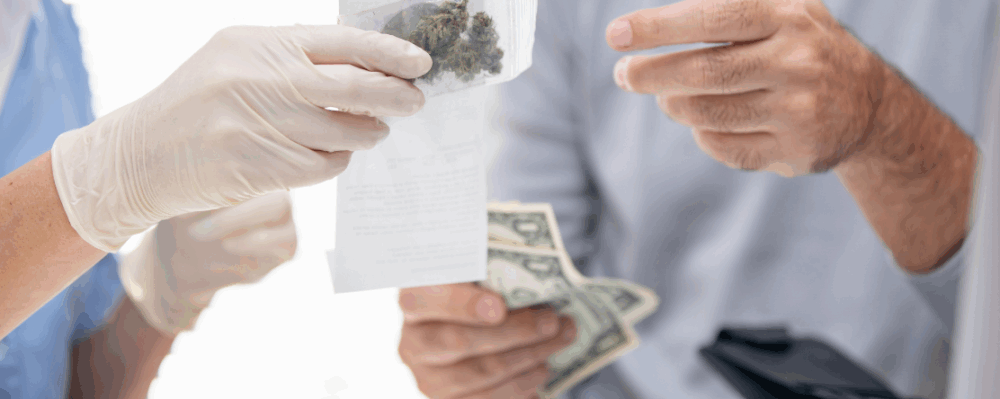
She knew that many people with substance use disorders land in the ER, and that starting medications for opioid use — like buprenorphine (often known by the brand name Suboxone) — could double a person’s chance of staying in treatment a month later.
Yet she also knew that providing the medication was far from standard practice.
Daniel Browne started drinking alcohol and using prescription opioids at age 14. By the time he was 24, he was on the verge of losing his job, his car and his apartment.
“I didn’t know where else to go to get treatment other than the ER,” he says.
In May 2020, Browne drove 15 minutes from his home to Adventist Health Howard Memorial Hospital in Willits, Calif., where he was immediately met by Mary Anne Cox Gould. At the time, Cox Gould was a substance use navigator for a program called CA Bridge. She championed addiction treatment in the hospital and helped connect patients from the ER to clinics in the community. (Cox Gould is now a supervisor of other navigators in Adventist Health hospitals.
“She met me in the parking lot even before I went into the ER,” Browne recalls.
She stayed with him as he received his first dose of buprenorphine, which provided immediate relief from withdrawal symptoms. “Once you’re not facing the crippling detoxification, it’s much easier to not relapse,” Browne says.
Cox Gould then walked him over to the hospital’s outpatient clinic and helped him schedule recurring appointments. When Browne ran into obstacles filling his buprenorphine prescription at a local pharmacy, she made the necessary arrangements for him to get it from the hospital pharmacy, instead.
Now more than a year into recovery, Browne says he’s become a more reliable employee and has reconnected with his parents and younger brother — successes he credits partly to the medication and consistent support he’s received.
Those are hallmarks of the CA Bridge program, says executive director Serena Clayton. Medication is considered a key element of treatment. Connecting patients with a navigator helps them in long-term recovery. And having navigators in the ER creates a more welcoming environment for patients, and gives ER staff a chance to learn more about addiction, she says.
The model is currently used by about 130 hospitals in California, and the state has allotted $40 million to expand the program to more than 100 others. The funds cover the salaries of substance use navigators, training for ER staff on prescribing buprenorphine and other technical assistance.

This doesn't have to be a one-off story about a really special hospital. It can happen at scale.Serena Clayton, CA Bridge
Click below to see the full story from NPR.
Originally published by NPR
More Updates
Work With Us
You change the world. We do the rest. Explore fiscal sponsorship at PHI.
Support Us
Together, we can accelerate our response to public health’s most critical issues.
Find Employment
Begin your career at the Public Health Institute.



