
California Pregnancy-Associated Mortality Review: California Pregnancy-Related Deaths, 2008-2016
- Christy McCain, MPH
- Paula Krakowiak, Dan Sun, David Reynen, Diana Ramos, Shabbir Ahmad, Romeo Amian, Connie Mitchell, Elliott K. Main, Christine H. Morton, Delphina Alvarez
-
Focus Areas
Women, Youth & Children -
Issues
Reproductive & Sexual Health -
Expertise
Research – Quantitative -
Programs
California Pregnancy-Associated Mortality Review

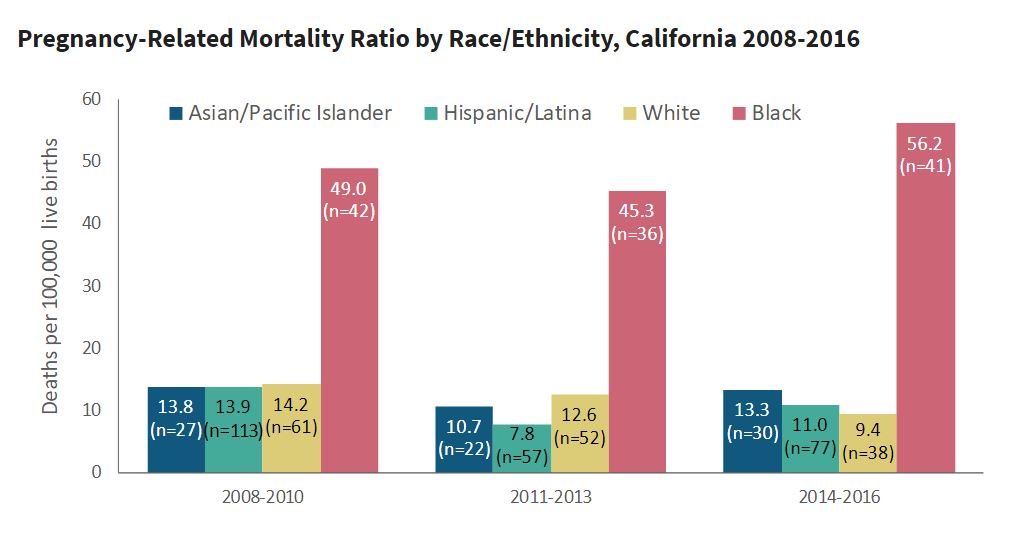
Released in September 2021, a California Pregnancy Mortality Surveillance System (CA-PMSS) report finds that California’s rate of pregnancy-related deaths has remained low compared with the U.S. rate and has been largely stable from 2008 to 2016. However, racial/ethnic disparities in pregnancy-related mortality ratios appear to be worsening, particularly among Black women. Black women were overrepresented among pregnancy-related deaths from all causes, especially deaths that occurred in pregnancy prior to birth or after delivery hospitalization.
While California has made progress to reduce maternal mortality through investment in maternal health programs, strong leadership and engagement of the maternity care community and targeted hospital quality improvement, more needs to be done to narrow racial/ethnic disparities.
See the reportThe California Pregnancy Mortality Surveillance System (CA-PMSS) is a statewide surveillance of deaths among Californians who were pregnant within the prior year. Funded by the federal Title V Maternal and Child Health Block Grant, the Maternal, Child and Adolescent Health (MCAH) Division of the California Department of Public Health (CDPH) initiated CA-PMSS and relies on a collaboration with three key partners: The Public Health Institute, Stanford University’s California Maternal Quality Care Collaborative, and a volunteer review committee of experts.
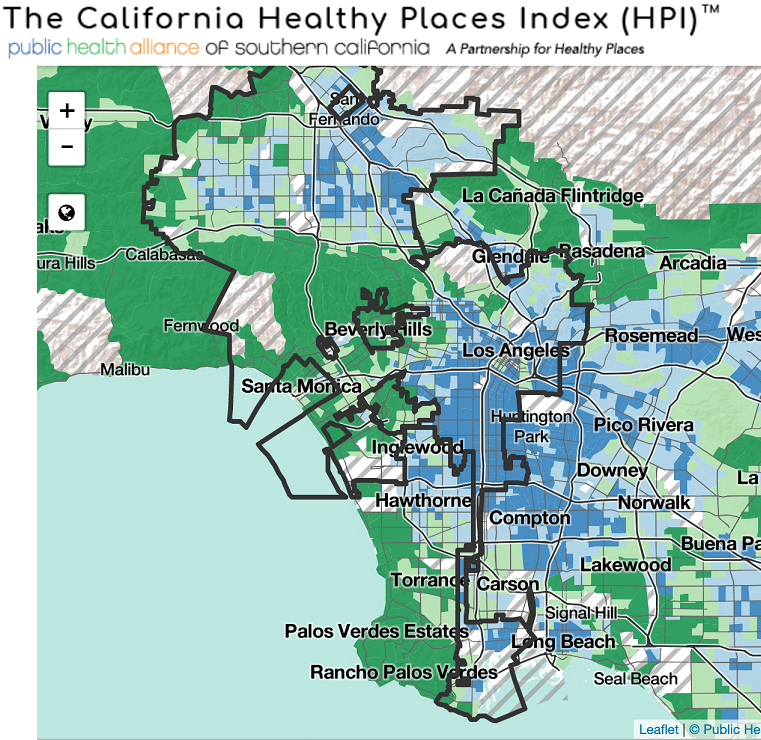
Social Determinants of Health & Pregnancy-related Mortality: Using the Healthy Places Index
Pregnancy-related mortality was examined within the context of social determinants of health by incorporating the California Healthy Places Index, a validated measure of community well-being created by PHI's Public Health Alliance of Southern California. The HPI provides overall scores and more detailed data on specific policy action areas that shape health, like housing, transportation, education and more. California is among the first in the nation to include a validated measure of community conditions in the analysis of pregnancy-related mortality.
Explore key findings from the report:
Pregnancy-related deaths in California:
- In 2008-2016, 1,934 women died while pregnant or within one year of the end of a pregnancy; 31% (608) of these deaths were related to pregnancy or its management.
- California’s annual pregnancy-related mortality ratios remained low and largely stable in 2008-2016, fluctuating between 9.5 and 14.9 deaths per 100,000 live births. One exception was a spike in pregnancy-related deaths caused by influenza A (H1N1) during the 2009 pandemic, which resulted in an elevated pregnancy-related mortality ratio of 17.1 in 2009.
By cause and timing to death:
- The top five leading causes of pregnancy-related deaths were cardiovascular disease (28%), sepsis or infection (17%), hemorrhage (15%), hypertensive disorders (13%) and thrombotic pulmonary embolism (7%).
- Eighteen percent (18%) of pregnancy-related deaths occurred while pregnant, and of the remaining 82% that occurred after pregnancy ended, nearly half (44%) of the deaths were within six days of childbirth (or end of pregnancy), 24% occurred 7-42 days after pregnancy ended and 14% were 43-365 days after pregnancy. Timing to death varied greatly depending on the cause of death.
By sociodemographic and place-based characteristics:
- Pregnancy-related mortality ratios were elevated for women with the following characteristics: older age (35 years or older), pre-pregnancy obesity (body mass index 30 or greater), public insurance (e.g., Medi-Cal) and no high school diploma.
- The pregnancy-related mortality ratio was highest for women living in the least advantaged communities (16.4 deaths per 100,000 live births), more than twice the mortality ratio for women living in the most advantaged communities (6.8).
- Pregnancy-related mortality ratios varied by geographic region, from 10.8 to 17.8 deaths per 100,000 live births; the Southern Central Valley region (includes Fresno, Kern, Kings, Madera, Mariposa, Merced, Stanislaus, Tulare and Tuolumne counties) had the highest pregnancy related mortality ratio of 17.8.
By race/ethnicity:
- Racial/ethnic disparities in pregnancy-related mortality ratios widened between 2008 and 2016. From 2014-2016, the pregnancy-related mortality ratio for Black women was 56.2 deaths per 100,000 live births, four to six times greater than the mortality ratios for women of other racial/ethnic groups including White (9.4), Hispanic (11.0) and Asian/Pacific Islander (13.3).
- Black women were overrepresented among pregnancy-related deaths from all causes, especially deaths that occurred in pregnancy prior to birth or after delivery hospitalization (7-42 days and 43-365 days after pregnancy ended).Hispanic/Latina women were the least likely to die during pregnancy or the late post-pregnancy periods.
Originally published by The California Pregnancy Mortality Surveillance System
Work With Us
You change the world. We do the rest. Explore fiscal sponsorship at PHI.
Support Us
Together, we can accelerate our response to public health’s most critical issues.
Find Employment
Begin your career at the Public Health Institute.


