
In the News
Can Something This Simple Save the Lives of Drug Users?
- Orange County Register
-
Focus Areas
Alcohol, Tobacco, Drugs & Mental Health -
Issues
Rural Health -
Expertise
Outreach & Dissemination -
Programs
CA Bridge
Substance users who come to hospital emergency departments are typically stabilized and then handed a “street sheet,” a list of phone numbers for 12-step programs and treatment centers. But now that may be about to change.
As drug deaths rise to historic highs in California — from 2018 to 2019 opioid deaths shot up 27% and deaths from all drugs rose 10% — the state is pumping $20 million into a simple idea that promises a fundamental shift: Deliver medication to treat addiction while patients are still in the the emergency room, and use an on-staff “substance use navigator” to back that up. The navigator can then shepherd users into follow-up care to help them stay on track.
The Behavioral Health Pilot Project is based on the CA Bridge program of addiction treatment that’s been piloted in 52 acute-care hospitals, and is part of California’s pivot away from a largely unregulated, problem-plagued, behavior-based approach overseen by former users to a scientific, medical model overseen by physicians.
The grants are not for earth-shattering gobs of money — most hospitals are getting $100,000 to pay for that “navigator” — but the shift in attitude that they represent is huge.
“The money, for a hospital, is just a drop in the bucket. What’s changing is the standard of care. Traditionally, hospitals didn’t see themselves as treating substance use disorder. That was done in outpatient care, in clinics. But this is really a sea change. Sometimes, the hospital emergency room is the only place where these patients come into contact with the medical care system. They’re in crisis, and there’s a moment — an open door — where patients are most open to getting treatment.” Skye Christensen, spokesperson for CA Bridge.
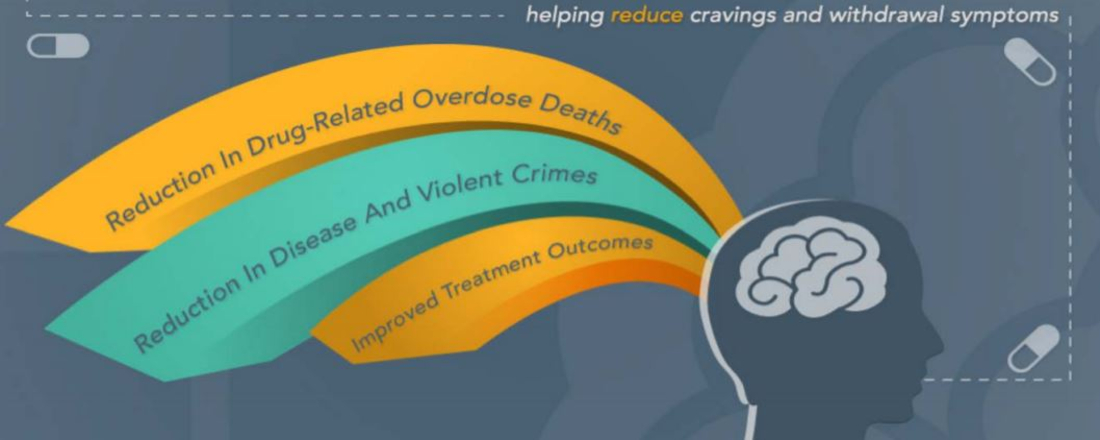
As hospitals and emergency departments become primary access points for treatment, under the CA Bridge model patients immediately begin medication-assisted treatment with drugs like buprenorphine, which binds to the brain’s opioid receptors and blunts opioid highs. Hospitals also distribute the overdose-reversing drug naloxone to minimize the risk of overdose death. Hospitals must have on staff a licensed mental health professional or substance use disorder counselor registered with, or certified by, a professional organization approved by DHCS, who follows up with patients and guides them into evidence-based treatment.
Based on the work piloted by the California Health Care Foundation, the state Department of Health Care Services tapped Medication Assisted Treatment Expansion Project funding to launch the program in March 2018, and contracted with the Public Health Institute in October 2018 to expand the system to 52 hospitals, said DHCS spokesperson Carol Sloan.
Performance data from the state show that, in its first year, 52 health care facilities across 35 counties initiated medication-assisted treatment and referred 2,060 individuals into treatment. The program also provided recovery services through referrals to 4,302 clients.
The state’s broader MAT efforts for Sept. 30, 2018 through September 29, 2019 show that a total of:
- 7,381 people received treatment services through projects like CA Bridge.
- Of those, 1,806 received methadone; 5,144 received buprenorphine; and 431 received injectable naltrexone.
- The number of clients receiving recovery support services was 7,875.
The big message is, ‘Substance use disorder is a chronic illness. It’s a medical problem and yes, it can be treated medically....It’s transformative. It’s not a heavy lift. With a small investment you can leverage a lot of your existing resources to reach a broad population and save lives.Dr. Aimee Moulin, co-principal investigator at CA Bridge and behavioral health director for the UC Davis Medical Center’s emergency department
Click below to read the full article in the Orange County Register.
Originally published by Orange County Register
More Updates
Work With Us
You change the world. We do the rest. Explore fiscal sponsorship at PHI.
Support Us
Together, we can accelerate our response to public health’s most critical issues.
Find Employment
Begin your career at the Public Health Institute.



