PHI Impacts 2020
In January of 2020, we could not have imagined that the world would be facing a devastating pandemic exacerbated by a vulnerable healthcare system, a polarized political and social landscape and an economic downturn of historic proportions. COVID-19 has amplified the reality of systemic racism nationally and globally. It has put a spotlight directly on the challenge of health equity and the need for immediate steps toward racial justice to mitigate the deadly disproportionate impact for communities that are primarily Black, Indigenous and people of color.
Throughout its 56-year history, PHI has been a national leader and partner in addressing some of the most complex public health issues of our generation. We moved through those difficult moments in history with our resilience, creativity and unflinching commitment to improving the health, well-being and quality of life for individuals and communities around the world.
2020 was no exception. I invite you to read through some of the landmark moments in this unprecedented year, and see how PHI and its programs stood throughout: for health, justice and equity.
Mary A. Pittman, DrPH
CEO & President
Public Health Institute

LIsten to PHI’s CEO Mary Pittman explain how PHI addressed equity and interrupted the spread of COVID-19 in 2020.
Leveraging Infrastructure and Expertise to Distribute PPE and to Promote Telehealth
In March of 2020, PHI joined schools, businesses, government agencies and other non-profits in moving most of its work to remote operations. When COVID-19 restrictions began, PHI stepped in to provide immediate public health guidance to help deliver PPE to where it was most needed, in a matter of days. With the urgent need to protect patients and health care providers, telehealth became a key strategy for many health care systems. PHI’s Center for Connected Health Policy (CCHP), the federally designated National Telehealth Policy Resource Center, worked for more than a decade to expand access to telehealth, laying the groundwork for telehealth coverage and policy changes. State and federal government began implementing CCHP policy and funding recommendations. During the pandemic, CCHP became a guiding voice for the implementation, interpretation and next steps necessary for telehealth law and accessibility, issuing a series of detailed explainer videos. Riley Wagner, MPH, who is a PHI/CDC Global Program Management Fellow for CDC’s Center for Global Health Headquarters in Atlanta, was the first of thirty-four PHI/CDC fellows to be assigned to CDC’s Emergency Operations Center in response to the COVID-19 pandemic. Riley worked on the Cruise Ship Task Force that was the source of the first major U.S. outbreak. Beginning in May, PHI’s Sustaining Technical and Analytic Resources provided global technical assistance focused on ventilator deployment, critical care capacity assessments, and critical care education. Their work helped support USAID partners supply over 10,000 ventilators to more than 40 low- and middle-income countries.
Scaling a Contact Tracing Workforce: From Communities; for Communities
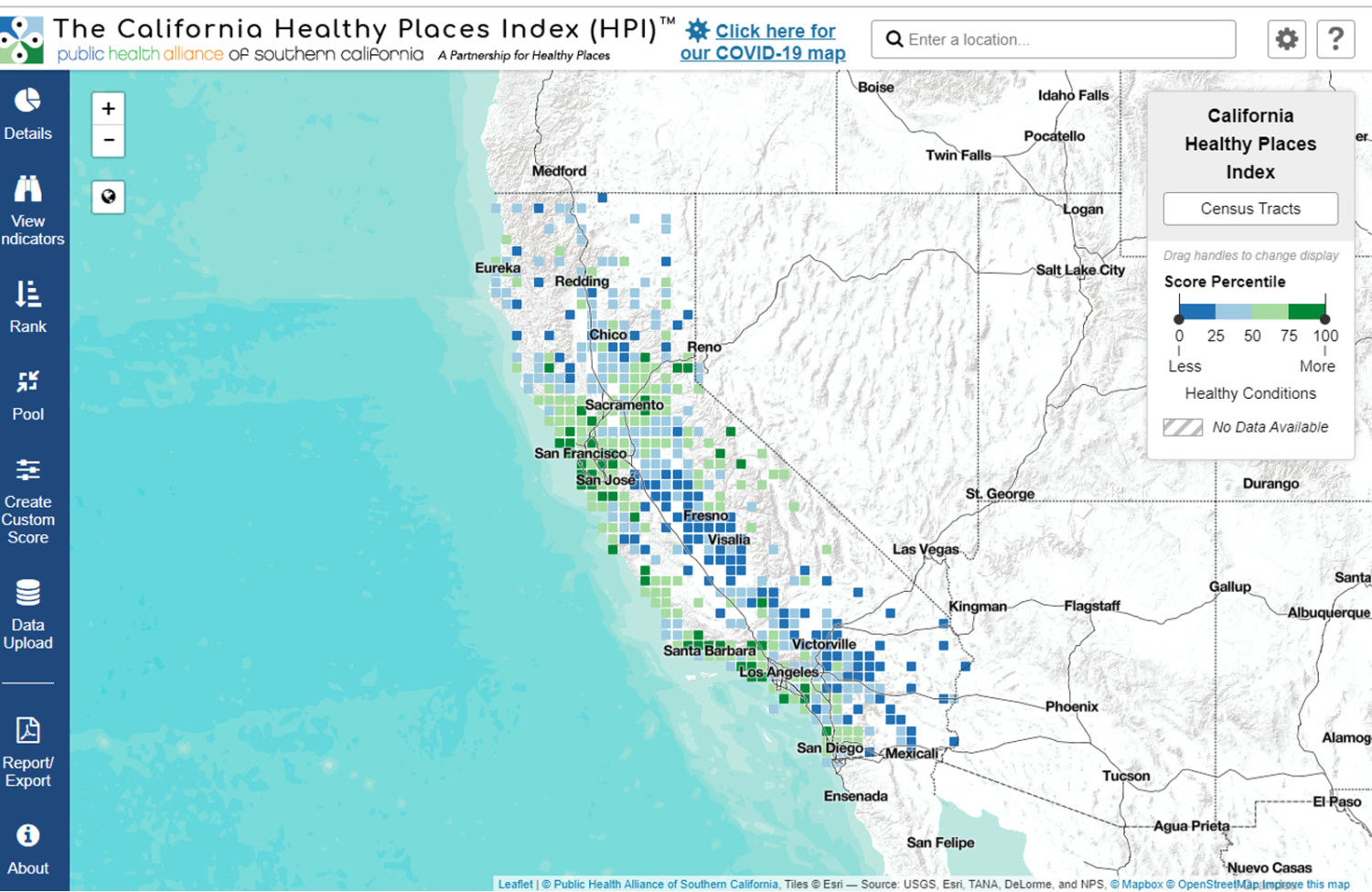
As the urgency of the COVID-19 pandemic became apparent, PHI’s central operations team was able to sign contracts and hire staff in just a matter of a few business days, to launch the contact tracing initiative, Tracing Health, in Oregon and Washington. In partnership with the Oregon Public Health Institute, the PHI team quickly addressed and quelled early outbreaks in the area and scaled the successful work rapidly. The Tracing Health model was designed to hire directly from impacted communities—creating jobs, engaging trusted messengers and building a >75% bilingual healthcare workforce to outlast the pandemic. To address the systemic inequities and structural racism that lead to disproportionate transmission cases and death rates in Black and brown communities, PHI embedded an equity lens into each of our COVID-19 initiatives, including hiring directly from communities and providing workforce development, building trust and equity in contact tracing, tracking environmental and health disparities to strengthen resilience before the next crisis, addressing discrimination and racism and connecting data to larger systemic inequities. Building on its successful approach to contact tracing in the Northwest U.S., PHI and its programs worked rapidly to expand its COVID-19 work. In August, PHI was able to increase its capacity in California through a partnership with Kaiser Permanente to support contact tracing efforts. The Public Health Alliance of Southern California’s Healthy Places Index (HPI) provided data to drive a statewide California COVID-19 Health Equity Metric, and their COVID-19 Equity Snapshot series provided resources to showcase the power of public health in response to the COVID-19 crisis.
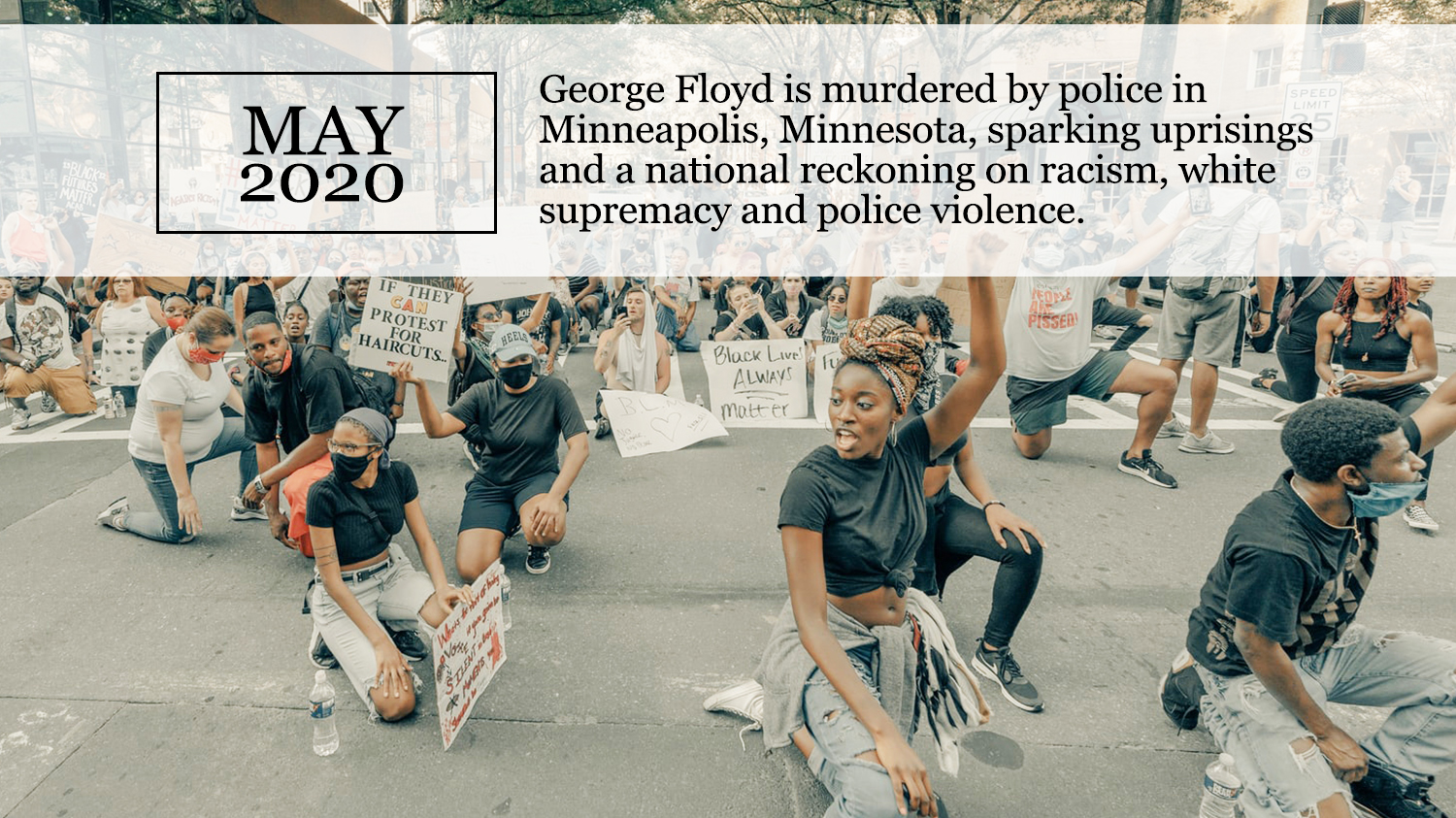
Working to End Systemic Racism
PHI recognizes that racism is a public health issue and embeds racial justice and health equity across our work. In the wake of George Floyd’s murder, PHI stood in solidarity with Black leaders and communities in calling for justice and action to end police violence. Amidst calls to defund police, PHI programs released two briefs: our Berkeley Media Studies Group published “Public Health Over Punishment: Media tools for communicating about police and prison budgets,” and our Getting it Right from the Start program released “California Cannabis Tax Revenues: A Windfall for Law Enforcement or an Opportunity for Healing Communities?” PHI continued our organizational work to address racism, including deepening an already-in-process Diversity, Equity and Inclusion initiative. PHI’s CA4Health program launched its first two Racial Equity & Social Justice 21-Day Challenges for staff and partners, which explored the history of racism and discrimination to build more effective social justice. PHI president and chief executive officer Mary Pittman was selected by the University of California Berkeley School of Public Health as one of sixteen public health women leaders, for her work in addressing health inequities.
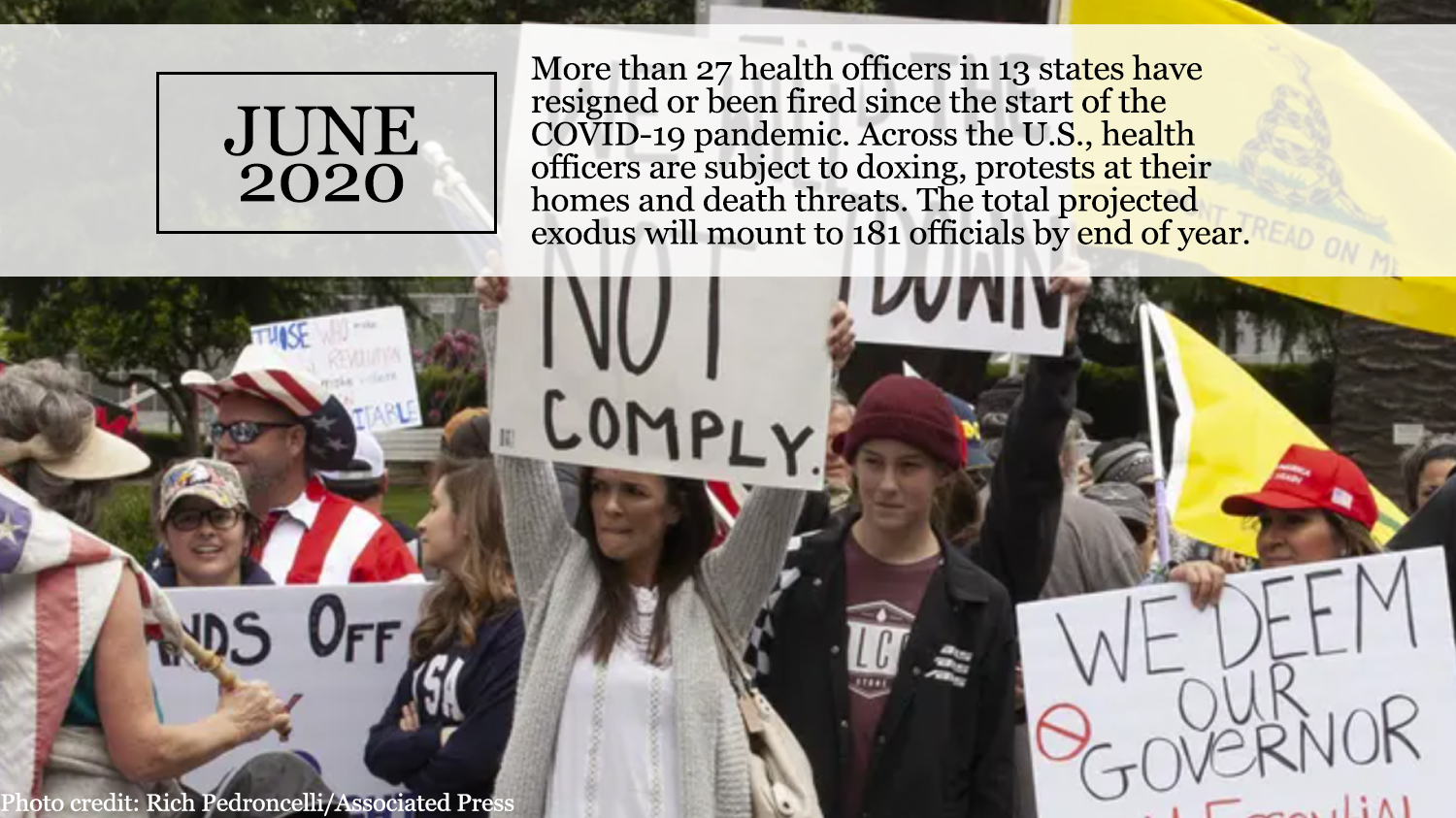
Leading the Call to Protect Science and Public Health
The COVID-19 pandemic called for brave leadership, accurate information and clear voices in support of the principles of public health. As public health officials received death threats for making science-based recommendations to contain the virus, PHI stood by their side, saying, “Instead of bulletproof vests and security details, our local public health officials deserve the protection of those who appointed them, and of those they serve.” When the CDC quietly made revisions to their COVID-19 testing guidelines that contradicted evidence-based guidance, PHI and partners successfully mobilized 250 organizations to call for a reversal of the guidelines. In The New York Times, PHI president and chief executive officer Mary Pittman stated, “It is critical that science, evidence and data continue to serve as the foundation of every CDC recommendation.” In response to the Administration’s embrace of a “herd immunity” approach to the COVID-19 pandemic, PHI joined other leading national health organizations in a statement warning that the approach would lead to a greater risk of severe disease and deaths.
Connecting Wildfires, Climate Change and Social Determinants of Health
Wildfires, record-breaking heat waves and air pollution ravaged the West Coast, but not everyone was affected equally. After more than a decade of work connecting climate change, environmental justice, health and equity, PHI’s experts were prepared to share their knowledge on how underlying disparities in environmental and health conditions exacerbate vulnerability during public health emergencies in low-income communities and communities of color, and the possible long-term effects of inhaling wildfire smoke. PHI’s Gina Solomon and our Tracking California program are investigating the role that race and air pollution may play in the COVID-19 crisis in communities of color. As part of Listos Calfornia, a statewide disaster preparedness campaign, the Center on Disability at the Public Health Institute engaged more than 300,000 vulnerable residents in three California counties. They created a planning tool, “4 Steps to Emergency Preparedness for All,” to help individuals prepare for emergencies and contributed to materials and videos that included and addressed the emergency preparedness needs of people with disabilities, seniors and older adults and people in poverty.
PHI took a stance to support Governor Newsom’s climate change order and called for more action at the federal level. When the Trump Administration officially withdrew from the Paris Climate Accord on the day after Election Day, PHI reiterated our support for climate science, noting that, “[T]he U.S. has a critical role to play in addressing climate change and must fully engage—and lead—on efforts to address and mitigate the crisis.”
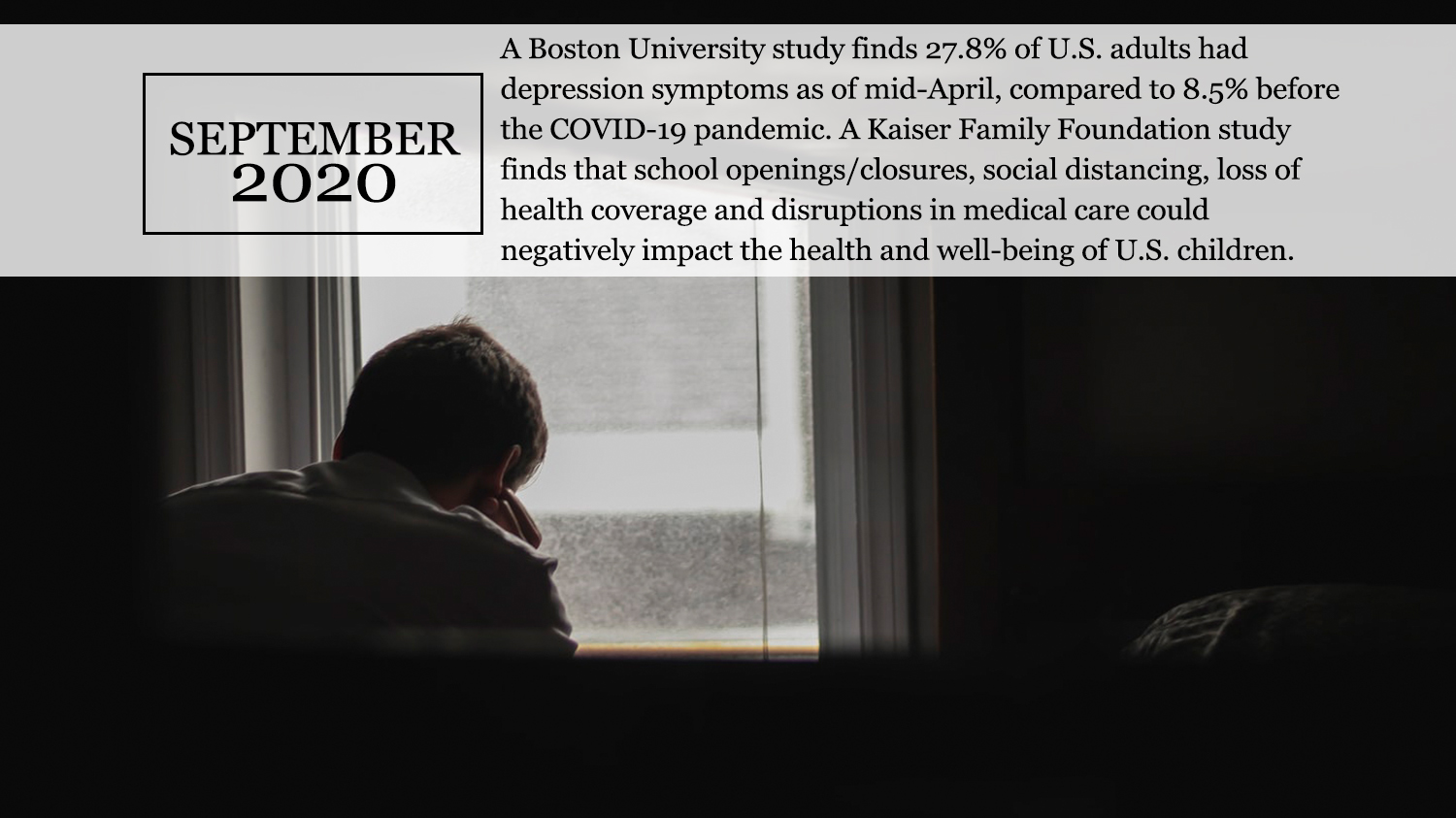
Addressing Childhood Stress and Mental Health Needs
Isolation, anxiety, financial stressors and other COVID-19 related factors had profound impacts on mental health in 2020. In order to address these issues across the communities that we work with, PHI deepened its work in both trauma-informed care and in mental health first aid. Trainings on these topics were offered online and are now part of trainings for PHI’s contact tracers, so that they are more able to identify and support both the mental and physical needs of those they work with. “We had a suicide prevention training just days before we had our first contact who was considering suicide,” said Nafisa Fai, a contact tracing team manager at Tracing Health. Experts also worried whether distance learning could also shut down the child abuse reporting channels that help keep children safe. PHI’s Northern ACEs Summit brought together experts in Adverse Child Experiences, or ACEs, including California Surgeon General Nadine Burke Harris, to identify and address all of the factors connected to childhood—and lifelong—health, and with our partners at IMPAQ we addressed mental health first aid in schools. Our Build Healthy Places Network released a series of fact sheets aimed to highlight the role of community development in addressing mental health, social isolation and homelessness.
Creating New Paths to Treat Substance Use
When the COVID-19 pandemic hit, a collision of two epidemics created a spike in opioid use: more than forty states reported increases in opioid overdose deaths. PHI’s CA Bridge program responded, creating new guidance and collecting resources for health care workers on treating opioid use while minimizing the risk of COVID-19 transmission. In August, the state recognized the vital work of CA Bridge with a $20 million pilot project to bring the CA Bridge model to more than 200 hospitals, about two-thirds of all hospitals in the state. PHI’s Center for Connected Health Policy (CCHP) also developed an analysis of policies needed to help clinics in rural and other underserved areas adopt telehealth for treating patients with opioid use disorder during COVID-19 and beyond. And, in December, PHI moved its groundbreaking cross-sector National Opioid Leadership summit online, bringing together criminal justice, medical and public health experts to share best practices, including during an epidemic.
Ending the Year with New Hope
As the first batch of vaccines were delivered across the country, the end of the pandemic finally came into sight. Yet December also marked the hardest part of the pandemic to date, as cases rapidly grew, ICU and hospital beds dwindled and care provision diminished. PHI expanded its contact tracing partnership across multiple counties in California, and Together Toward Health, a pooled fund created by thirteen major foundations, began issuing its first micro-grants to community-based organizations in California’s most impacted neighborhoods. Roots of Change and the Center for Wellness and Nutrition partnered with community-based organizations, tech companies, local government and grocery stores in some of California’s hardest hit communities, to distribute more than $20 million in food cash cards directly to those in greatest need, including families who do not qualify for or who are unable to access federal food programs. While continuing to address the immediate needs of suppressing COVID-19, PHI began to look to the future. PHI’s Safely Opening Schools, a pilot, on-site, rapid COVID-19 screening program, will screen all teachers, staff and students for COVID-19 one to two times per week with FDA-approved tests. By reducing the risk of COVID-19 transmission in schools, SOS aims to facilitate safer reopening, especially in African American and Latino communities and other school districts hardest hit by COVID-19. Recognizing the need to build community engagement and confidence in vaccines, PHI’s Berkeley Media Studies Group released “Communicating about the COVID-19 Vaccines: Guidance and Sample Messages for Public Health Practitioners.” In 2021, we turn again toward justice, health and hope.
Our Impact
- 10M in food vouchers distributed to families unable to receive other types of assistance
- 66K+ hours of contact tracing calls
- 164K people with disabilities and other socially vulnerable adults connected to COVID-19 resources

Work With Us
You change the world. We do the rest. Explore fiscal sponsorship at PHI.
Support Us
Together, we can accelerate our response to public health’s most critical issues.
Find Employment
Begin your career at the Public Health Institute.